You have not yet added any article to your bookmarks!

Join 10k+ people to get notified about new posts, news and tips.
Do not worry we don't spam!
Post by : Anis Farhan
Drug discovery is one of the most complex and expensive processes in modern science. Developing a single medicine can take more than a decade and billions of dollars, yet failure rates remain incredibly high once drugs reach human trials. For decades, pharmaceutical companies have relied heavily on animal testing to predict how new drugs will behave in humans. However, animal physiology often differs significantly from human biology, leading to inaccurate predictions, safety risks and wasted research investment.
This is where Human Organs-on-Chips—micro-engineered biological models that mimic human organ function—are changing the game. Designed to recreate the structure and physiological behavior of human tissues, these devices offer a groundbreaking way to test drugs safely, efficiently and ethically. In recent years, they have moved from futuristic prototypes to practical tools used by researchers, biotech innovators and even regulatory bodies.
Organs-on-chips promise a revolution in drug testing: a world where scientists can predict human responses with far greater accuracy, reduce reliance on animal studies and accelerate the journey from lab discovery to real-life treatment.
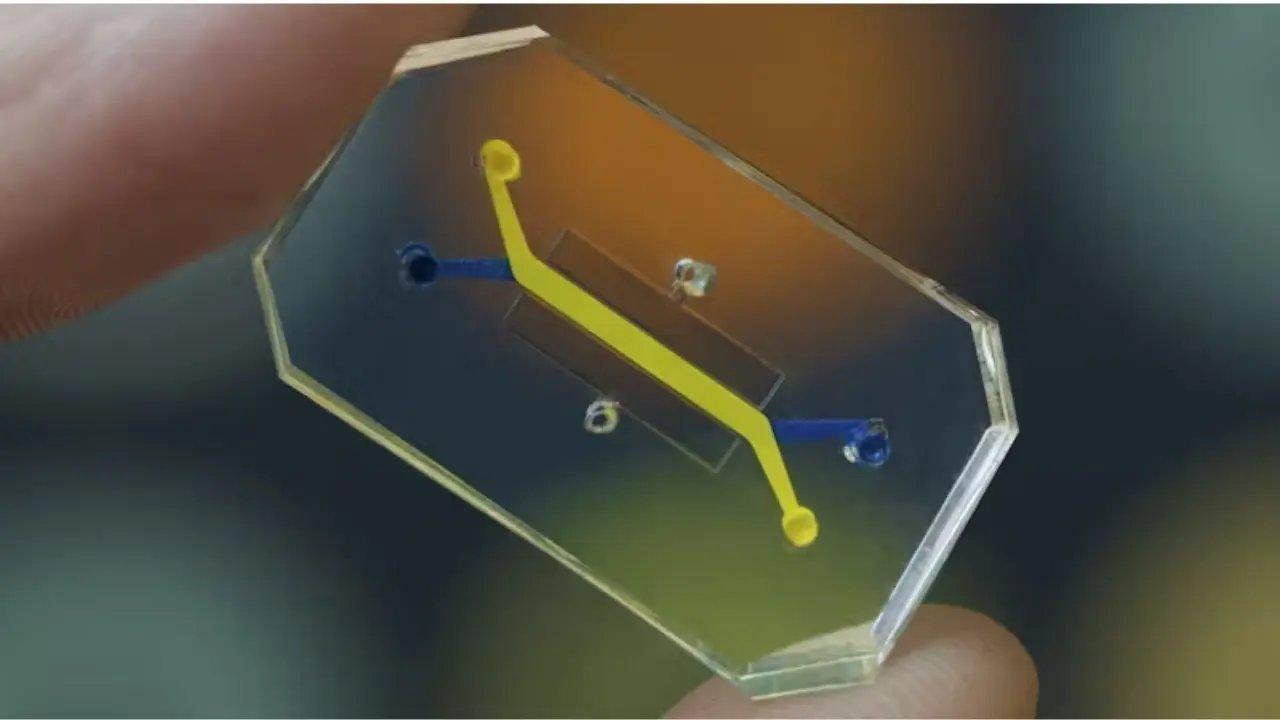
An organ-on-chip is a small, transparent device—often no larger than a USB drive—containing tiny channels lined with living human cells. These cells are arranged in patterns resembling human tissues, allowing the device to perform organ-level functions.
In essence, these chips combine:
cell biology
tissue engineering
microfluidics (precise manipulation of tiny amounts of fluids)
biomechanics
Together, these elements recreate a human organ’s natural environment, including blood flow, mechanical forces and chemical exposure.
Organs-on-chips can model:
lungs expanding and contracting
heart tissues beating
intestinal tissues absorbing nutrients
liver cells metabolizing drugs
kidney cells filtering toxins
This dynamic nature sets them apart from flat laboratory cell cultures, making them much more accurate and predictive.
Animal testing has long been controversial and scientifically flawed. Many drugs that appear safe in animals later fail in humans due to physiological differences. Organs-on-chips, however, use real human cells and mimic human physiology, offering far more accurate predictions of:
toxicity
drug absorption
metabolism
side effects
organ-specific responses
This could significantly reduce the failure rates in clinical trials while minimizing ethical concerns.
Drug development can cost upward of two billion dollars. Much of that cost comes from failures in early or mid-stage trials. By using organs-on-chips to catch problems earlier, companies save:
time
money
human risk
resources
The ability to simulate human responses without immediately entering clinical trials is a powerful advantage.
Traditional models struggle to replicate:
rare diseases
genetic disorders
personalized health conditions
Organs-on-chips can be engineered using patient-derived cells. This allows for:
personalized medicine
drug testing tailored to an individual’s genetic makeup
modelling rare diseases impossible to replicate in animals
This technology opens the door to treatments once considered too complex or costly to develop.
The chip’s internal channels allow fluids to flow just like blood moves through the human body. This constant flow exposes tissues to nutrients, drugs and mechanical forces, enabling realistic organ behavior.
Organs such as lungs and intestines constantly experience motion. Organs-on-chips recreate these forces by stretching and compressing tissues in real time. This level of realism adds extraordinary accuracy to drug response predictions.
The chips are transparent, allowing scientists to observe biological responses instantly. This includes:
cell reactions
tissue damage
inflammatory responses
drug absorption patterns
Such real-time visibility has never been possible using animal models or traditional cultures.
One of the earliest breakthroughs, the lung-on-chip models the rhythmic expansion of human lungs. It has been used to study:
respiratory infections
environmental pollutants
asthma
drug toxicity affecting lung tissues
Its accuracy has led to collaborations between academic institutions, biotech companies and regulatory authorities.
Cardiac chips simulate beating heart tissues, allowing researchers to test:
heart drug toxicity
arrhythmia risk
metabolic pathways
effects of cancer treatments on heart cells
These chips are particularly valuable because cardiac toxicity is one of the top reasons drugs fail late in development.
The liver plays a crucial role in breaking down drugs. Liver chips help detect:
drug-induced liver injury
metabolic pathways
toxicity thresholds
enzyme interactions
This chip is considered vital in screening drugs that might cause liver failure.
The gut orchestrates digestion, immunity and microbiome interactions. These chips help scientists study:
nutrient absorption
gut diseases
inflammatory bowel disease
microbiome responses to medication
Such insights are extremely difficult to obtain using conventional laboratory models.
Kidneys filter waste and regulate fluid balance. A kidney chip helps researchers predict:
nephrotoxicity (kidney damage)
filtration rates
metabolic responses
Given that kidney toxicity is a major reason drugs fail, this model is highly impactful.
Organs-on-chips are helping researchers replicate conditions like:
cancer metastasis
viral infections
chronic inflammatory diseases
genetic disorders
This accelerates the search for new therapies and diagnostic solutions.
With increasing global restrictions on animal testing, cosmetic giants and chemical manufacturers are turning to chip-based human models. These chips allow companies to safely test:
skin irritation
chemical exposure
allergic reactions
without violating ethical guidelines.
Regulators are beginning to recognize the potential of organs-on-chips. They may soon become part of standardized drug approval pipelines, reducing reliance on animal data.
Eliminates or drastically reduces the need for animal testing. This aligns with global shifts toward cruelty-free research and ethical science.
Human-relevant data leads to better predictions, reducing failures in clinical trials.
Testing timelines shorten dramatically because scientists can run multiple simulations in parallel.
Each chip can be built with specific:
genetic profiles
disease conditions
environmental factors
This level of customization was previously impossible.
Despite its promise, organs-on-chips face several challenges:
Producing chips in large quantities remains expensive and technically complex.
While impressive, chips cannot yet replicate the full complexity of a human organ.
Researchers are still perfecting multi-organ chips that simulate an entire human body interacting in real time.
Although promising, most drug approval systems still rely heavily on animal data. Shifting to chip-based models requires major regulatory reform.
Scientists are now developing connected organ systems-on-chips, where multiple chips interact to mimic the entire human body. This opens the possibility of:
whole-body drug simulations
understanding how multiple organs respond together
identifying complications earlier
Eventually, integrated systems could model:
the immune system
metabolism
neurological responses
This futuristic approach brings us closer to a world where drug trials happen virtually before real humans are involved.
Human organs-on-chips represent one of the most significant shifts in biomedical research in decades. By providing human-relevant, ethically responsible and highly accurate models, this technology stands to transform drug testing forever.
As the world moves toward personalized medicine, reduced animal testing and faster therapeutic development, organs-on-chips emerge as a cornerstone technology that will shape the next generation of medical breakthroughs. Whether used for designing safer drugs, understanding complex diseases or predicting patient-specific outcomes, this innovation is paving the way for a smarter, more humane and more effective future in science.
Disclaimer:
This article is for informational and educational purposes and does not serve as medical or scientific advice.









Akshaye Khanna exits Drishyam 3; Jaideep Ahlawat steps in fast
Producer confirms Jaideep Ahlawat replaces Akshaye Khanna in Drishyam 3 after actor’s sudden exit ov

Kapil Sharma’s Kis Kisko Pyaar Karoon 2 to Re-release in January 2026
After limited screens affected its run, Kapil Sharma’s comedy film Kis Kisko Pyaar Karoon 2 will ret

Hrithik Roshan and Saba Azad Celebrate Christmas at Family Party
Hrithik Roshan and Saba Azad celebrated Christmas at Sussanne Khan’s party, sharing happy moments wi

China Sanctions 20 US Defense Firms Over Taiwan Arms Sales Dispute
China imposes sanctions on 20 US defense companies and 10 executives for supplying arms to Taiwan, e
Salman Khan’s Grand 60th Birthday Bash at Panvel Farmhouse Shines Bright
Salman Khan celebrates his 60th birthday with a grand party at Panvel farmhouse, sharing joyful mome

Thailand Defence Minister Joins Talks to End Deadly Border Clash
Thailand’s defence chief will join talks with Cambodia as border clashes stretch into a third week,