You have not yet added any article to your bookmarks!

Join 10k+ people to get notified about new posts, news and tips.
Do not worry we don't spam!
Post by : Anis Farhan
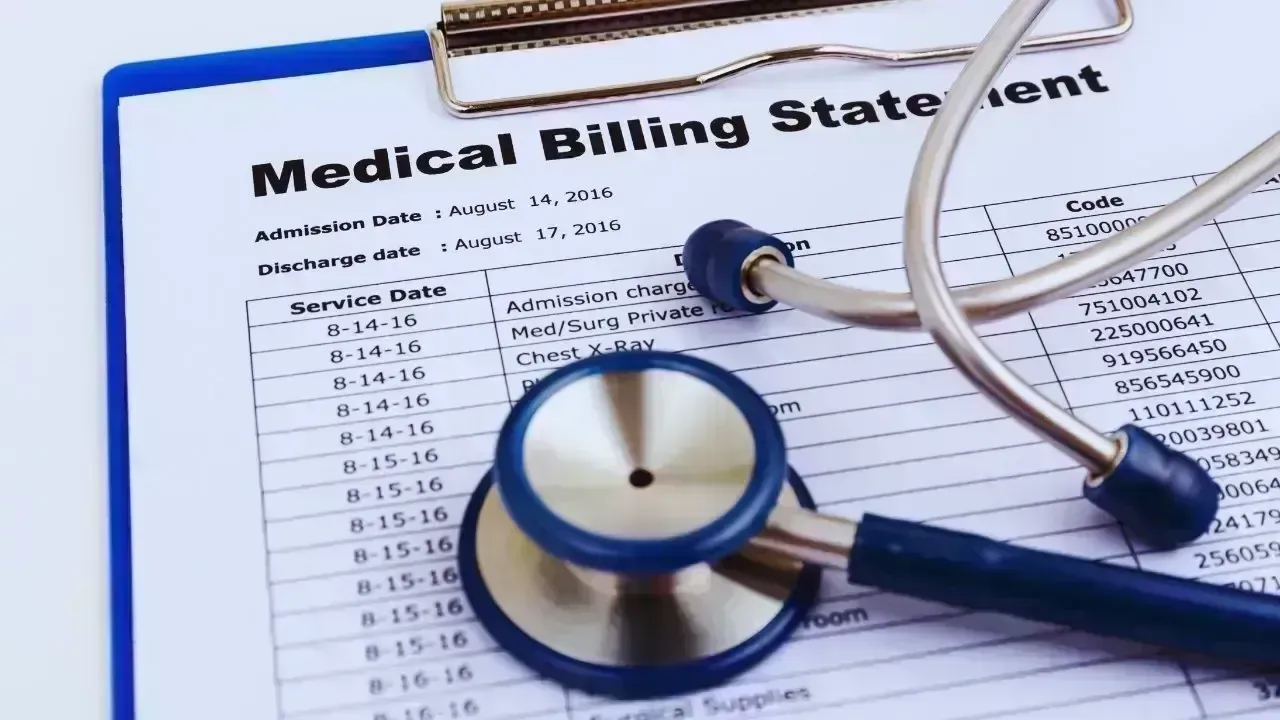
Historically, healthcare has been considered a fundamental right supported by society for communal wellbeing. Recently, however, it has evolved into a source of profound financial concern. By 2026, the surge in medical cost is not merely a theoretical policy issue; it has become a daily struggle for countless families.
From regular check-ups to crucial treatments, medical expenses have outstripped earnings in numerous regions. Even those with insurance are seeing their out-of-pocket costs escalate, while governments wrestle with the challenge of maintaining public health under strict budgetary constraints. This scenario creates a landscape where the affordability of care increasingly governs access rather than actual medical necessity.
A significant factor contributing to increased healthcare costs is medical inflation. Unlike general inflation, which affects everyday goods and services, medical inflation signifies the growing expenses related to medical services and treatments. In many regions, healthcare inflation consistently outpaces general inflation rates.
This divergence means that even modest wage increases make healthcare increasingly unaffordable. Families feel the strain through soaring insurance premiums and growing co-pays, along with skyrocketing prices for medical procedures and medications.
While medical advancements have saved numerous lives, they have simultaneously driven up costs. Sophisticated diagnostics and specialized treatments demand significant investment in technology and expert personnel.
These enhancements improve care but simultaneously inflate healthcare expenses. The challenge is evident: superior healthcare often results in higher financial burdens, leading to tough decisions for both patients and policymakers.
Even with insurance coverage, families face mounting direct costs related to healthcare. Deductibles, co-pays, and out-of-pocket expenses for uncovered services pile up quickly. Routine medical care that was once manageable now demands careful financial planning.
Middle-income families find themselves in a precarious position: earning too much for assistance but not enough to comfortably manage healthcare expenditures, making them susceptible to financial turmoil.
Healthcare costs are now a primary driver of household debt across many regions. An unexpected medical crisis can exhaust savings, compel families to borrow, or defer critical expenses like education and housing.
This pressure transcends individual patients, impacting families and often extending across generations.
Insurance is intended to provide financial security, but rising healthcare costs have led insurers to increase premiums and restrict coverage options. Many policies now offer less comprehensive benefits or mandate higher costs for policyholders.
Consequently, insurance often acts more as a partial barrier rather than full protection. Many hesitate to seek necessary care due to fear of high expenses.
Today's healthcare insurance systems are increasingly complex, complicating the understanding of what is and isn’t covered. This confusion can lead to unwelcome bills and delayed care, fostering skepticism towards the healthcare system.
Public healthcare systems are not shielded from surging costs. Governments are tasked with financing hospitals, staff, medications, and facilities—all while dealing with tight budgets.
As healthcare consumes a more significant portion of public funds, difficult decisions arise, such as cutting coverage, postponing essential developments, or shifting costs onto patients in the form of user fees.
An ageing demographic has led to a surge in healthcare demand, with older individuals requiring more frequent and complicated care, which places continual stress on public systems and drives costs higher annually.
The process of drug development is expensive, involving extensive research, testing, and regulatory requirements. Pharmaceutical companies maintain that high prices are necessary to subsidize innovation.
However, factors such as pricing strategies, patent protections, and limited competition frequently result in medicines that remain out of reach for many patients, leaving crucial drugs priced well beyond production costs.
The high costs of medications lead many individuals to ration their doses, postpone refills, or halt treatments altogether. Such actions not only deteriorate healthcare outcomes but also lead to greater expenses when previously manageable conditions escalate into emergencies.
While digital records and telehealth promise greater efficiency, they seldom come cheap. Upkeep, cybersecurity, and system improvements contribute substantially to overall healthcare costs.
Although technology can enhance care coordination, these financial benefits often require time to materialize, which maintains high short-term expenditures.
Healthcare systems are weighed down by multiple administrative layers linked to billing, compliance, and insurance processing. These non-clinical expenses siphon off considerable resources without directly improving patient care.
Ultimately, patients bear these additional costs through higher prices.
Soaring healthcare costs exacerbate existing inequalities. Affluent individuals often gain access to superior private care and faster services, whereas low-income populations face extended wait times or inadequate service.
This gap undermines the principle of equitable healthcare access, transforming it into a profit-driven system.
People living in rural or marginalized areas frequently face additional indirect costs such as travel, time off from work, and limited service availability. These factors further exacerbate financial challenges and deter timely access to care.
The financial anxiety stemming from healthcare expenses takes a toll on mental health. Concerns over bills, insurance coverage, and future medical costs add stress during vulnerable moments.
Such stresses can impede recovery and lead to long-term mental health issues.
The dread of medical costs causes many individuals to postpone or forgo necessary care. What begins as a mild issue might escalate into a critical health concern, raising both personal and financial costs.
Preventive measures such as vaccinations and health screenings can significantly lower long-term healthcare costs. Yet, such services remain undervalued and underused.
Neglecting preventive care leads healthcare systems to incur higher expenses later on due to emergency interventions and chronic disease management.
Both individuals and policymakers sometimes prioritize immediate savings, often at the expense of longer-term health investment. This practice may lower current spending but increase future healthcare expenses, maintaining the cycle of rising costs.
Patients directly face the costs through bills, premiums, and income loss. Families shoulder emotional and financial burdens, frequently making sacrifices to maintain care.
Healthcare expenditures reshape household priorities, influencing decisions about education, housing, and retirement.
Ultimately, public healthcare costs fall on taxpayers. With rising expenditures, governments may increase taxes, dial back other services, or accumulate debt.
The affordability of healthcare has consequently evolved into a critical issue that influences national policy and budget considerations.
Soaring healthcare costs hinder economic productivity. Poor health, deferred treatments, and financial strain reduce workforce participation and productivity.
Businesses grapple with mounting healthcare insurance expenses, while the economy suffers from slowed growth as healthcare becomes increasingly unaffordable.
Telemedicine holds the potential to lower costs through decreased hospital visits and improved access, presenting a convenient solution for routine check-ups.
Nonetheless, technology alone cannot resolve fundamental cost drivers such as pricing, administration, and demographic shifts.
Enhanced data management can lead to better care coordination and less redundancy. However, these improvements demand upfront costs and thorough systemic reform.
Certain governments deploy regulations to control medicine and treatment prices. While controversial, these measures can enhance affordability when appropriately applied.
The challenge resides in achieving a balance between cost management and maintaining quality and innovation.
Increasing healthcare accessibility frequently results in immediate cost increases. Sustainable savings hinge on effective management, prevention, and operational efficiency.
Decisions made today regarding policy will dictate whether healthcare remains accessible or becomes more exclusive.
Perceiving healthcare as an investment rather than merely a cost reshapes priorities. Healthier populations can contribute more effectively to society, curtailing long-term expenses.
This viewpoint bolsters a stronger focus on preventive measures and early intervention strategies.
Widespread demand for affordable healthcare often pressures political processes. Continued public advocacy is crucial for enacting meaningful reforms.
Ongoing structural factors—such as an ageing population, medical innovations, and chronic ailments—indicate that healthcare costs are unlikely to decrease rapidly.
The focus should shift from outright cost reduction to managing expenses in a fair and sustainable manner.
Success in healthcare systems is increasingly defined by affordability and access, alongside traditional health outcomes. Issues of equity and sustainability are emerging as central metrics.
The continual rise in healthcare costs is not merely a fiscal complication; it is a profound social concern. When individuals defer essential care, sacrifice basic needs, or endure anxiety regarding medical bills, the repercussions permeate families, communities, and economies.
In 2026, the pressing inquiry is no longer whether healthcare costs are escalating, but who bears the burden. Patients, families, governments, and society as a whole are impacted in multifaceted ways, necessitating comprehensive solutions rather than superficial fixes. A fundamental reevaluation of how healthcare is financed, delivered, and valued is imperative.
Ultimately, the real cost of healthcare encompasses more than monetary values; it also reflects the wellbeing, equity, and trust within society. The manner in which communities tackle this challenge will shape the health landscape for generations to come.
Disclaimer:
This article is intended for informational and analytical purposes only. It does not constitute medical, financial, or policy advice. Healthcare systems and costs vary by region and over time.










Rashmika Mandanna, Vijay Deverakonda Set to Marry on Feb 26
Rashmika Mandanna and Vijay Deverakonda are reportedly set to marry on February 26, 2026, in a priva

FIFA Stands by 2026 World Cup Ticket Prices Despite Fan Criticism
FIFA defends the high ticket prices for the 2026 World Cup, introducing a $60 tier to make matches m

Trump Claims He Ended India-Pakistan War, Faces Strong Denial
Donald Trump says he brokered the ceasefire between India and Pakistan and resolved eight wars, but

Two Telangana Women Die in California Road Accident, Families Seek Help
Two Telangana women pursuing Master's in the US died in a tragic California crash. Families urge gov
Ranveer Singh’s Dhurandhar Roars Past ₹1100 Cr Worldwide
Ranveer Singh’s Dhurandhar stays unstoppable in week four, crossing ₹1100 crore globally and overtak

Asian Stocks Surge as Dollar Dips, Silver Hits $80 Amid Rate Cut Hopes
Asian markets rally to six-week highs while silver breaks $80, driven by Federal Reserve rate cut ex